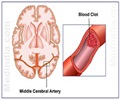
Daniel G. Hackam, M.D., Ph.D., from the University of Western Ontario, London, Ontario, Canada, and colleagues, conducted a retrospective study of six Canadian health care databases. They included 17,872 patients age 66 years and older who were admitted to Ontario hospitals for acute ischemic stroke from July 1994 to March 2008. Equal numbers of patients did not receive statins (control group) and did receive statins (intervention group). Patients were followed from 120 days after hospital discharge until they developed intracerebral hemorrhage (ICH), died or reached the March 31, 2010 endpoint of the study; the median (midpoint) follow-up time was 4.2 years.
Researchers found 213 episodes of ICH; the rate was slightly lower in patients treated with statins (2.94 vs. 3.71 episodes per 1,000 patient-years, respectively), but the difference was not statistically significant. Strokes were hemorrhagic in 10.09 percent of patients receiving statins and 10.23 percent of patients in the control group. Analysis of patient subgroups and statin dosage, and of screening tests that could indicate a healthy user bias or differences in quality of care, also did not demonstrate an association between medication use and ICH.
"At present, more than 80 percent of patients discharged from the hospital with a diagnosis of ischemic stroke are prescribed statin therapy," note the authors. "In a large North American jurisdiction, we found no evidence that such patients are at higher risk for cerebral bleeding than individuals who do not receive statins. Physicians should continue to adhere to current treatment guidelines recommending statin therapy for most patients with a history of ischemic stroke."
(Arch Neurol. Published online September 12, 2011. doi:10.1001/archneurol.2011.228. Available pre-embargo to the media at www.jamamedia.org.)
Editor's Note: This study was supported by a peer-reviewed grant-in-aid from the Physicians' Services Incorporated Foundation. Dr. Hackam and Dr. Kapral were supported by Canadian Institutes for Health Research New Investigator Awards. Dr. Austin was supported by a Career Investigator Award from the Heart and Stroke Foundation of Ontario. Dr. Kapral also receives support from the Canadian Stroke Network. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Advertisement
In an editorial, Philip B. Gorelick, M.D., M.P.H., from the University of Illinois College of Medicine, Chicago, discusses the results of the study by Hackam and colleagues in the context of other research about the effects of statin therapy on stroke and brain hemorrhage. "In clinical practice, the controversy over the administration of statins after stroke centers on the subsequent risk of brain hemorrhage in patients who might benefit from a reduction in major ischemic vascular events with statin therapy," he writes. Next, Gorelick outlines the results of other research addressing this question: "The HPS and SPARCL trial results suggest that there may be a signal of increased risk of brain hemorrhage with statin administration after stroke, whereas the Hackam et al findings diverge from this message." Gorelick suggests that differences in and limitations of the various study designs may help explain the discrepancy.
Advertisement
(Arch Neurol. Published online September 12, 2011. doi:10.1001/archneurol.2011.234. Available pre-embargo to the media at www.jamamedia.org.)
Editor's Note: Dr. Gorelick has served as a consultant to AstraZeneca and Pfizer. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Source-Eurekalert