‘A computer model developed to identify the parts of a person’s brain responsible for epileptic seizures may help in designing personalized surgical procedures.’
Tweet it Now
Researchers from the Newcastle University in England have developed a simulator that can analyze the nodes in brain of epileptic patients. The computer model can virtually predict the recurrence of seizures and the nodes in the brain responsible for the development of seizures.The software uses patients MRI scans to create a model that it can manipulate. The simulator mimics the removal of different nodes to see how they affect the activity in the rest of the network.
The researchers compared the response of targeting of commonly removed areas to those selected uniquely for each patient, showing a marked improvement in ability to fight seizures. But since this is still entirely a computer-based simulation, the researchers will have to compare the software against real patient cases to see whether it actually works.
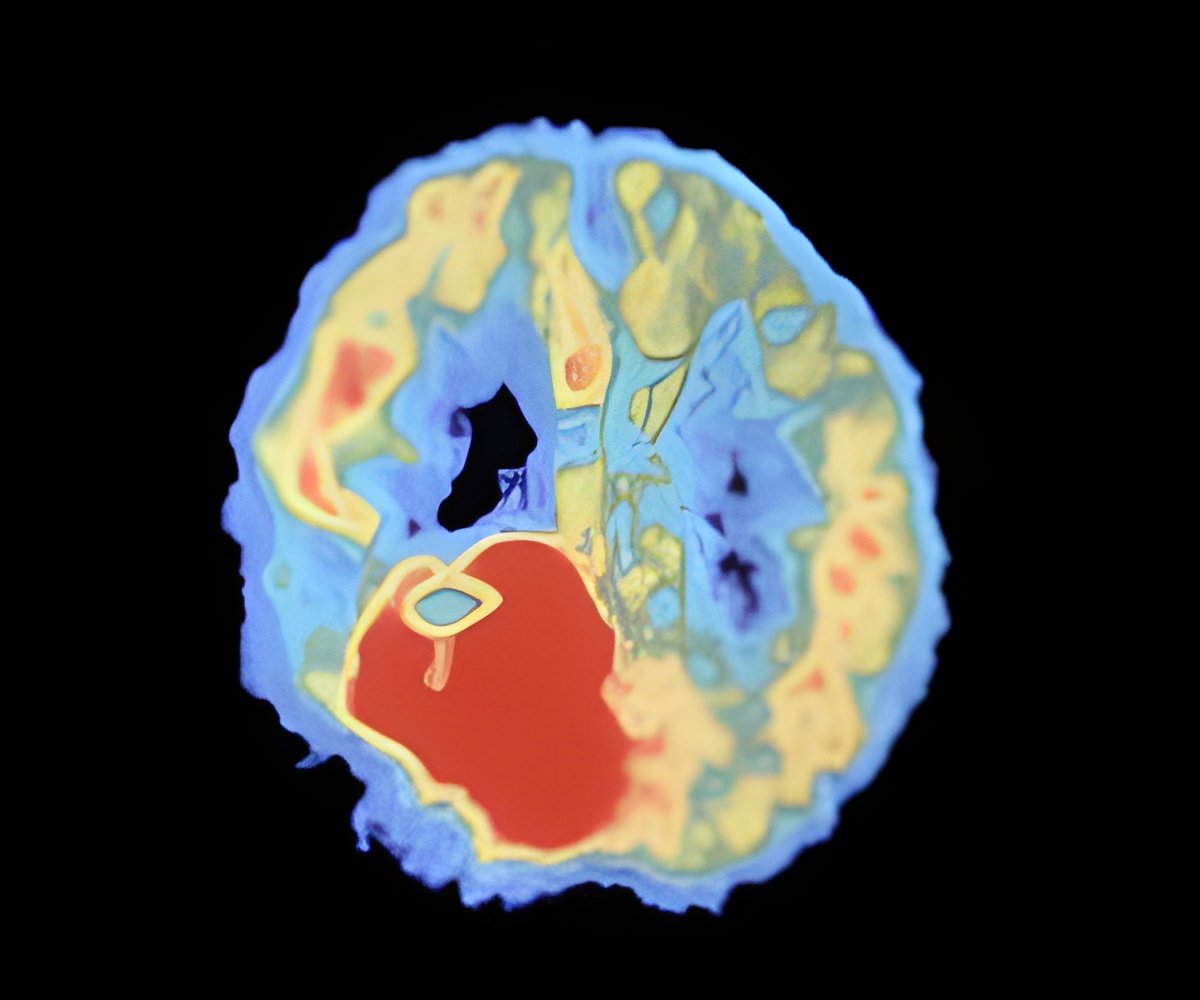
By simulating brain activity within each patient-specific network, they successfully identified regions that were more prone to seizures. The study is published in the Journal PLOS Computational Biology.
Researchers explained that patients tend to transit from non-epileptic to epileptic states more often than controls in the model. Regions in the left hemisphere (particularly within temporal and subcortical regions) that are known to be involved in TLE are the most frequent starting points for seizures in patients in the model. The model predicts that patient-specific surgery may lead to better outcomes than the currently used routine clinical procedure.
Advertisement
Research lead, Frances Hutchings added: “Removal of brain tissue is often the final option for treatment of temporal lobe epilepsy but we know that it is not always effective. It’s early days and there is more work to be done, but this model could assist surgeons in targeting surgical procedures more effectively and help people with epilepsy lead a more normal life.”
Advertisement
Source-Medindia