New clinical practice guidelines have been issued for diagnosing lymphangioleiomyomatosis (LAM) and managing pneumothoraces in patients with LAM, reveals a new study.
The guidelines have been published by the American Thoracic Society (ATS) and the Japanese Respiratory Society (JRS). The latest guidelines supplement LAM guidelines that the two societies issued in 2016 for the diagnosis and management of the rare lung disease that primarily affects women of child-bearing age. The latest guidelines are published in the American Thoracic Society's
American Journal of Respiratory and Critical Care Medicine.‘New guidelines aid in protecting patients with Lymphangioleiomyomatosis (LAM) from unnecessary drug exposures or surgical procedures and recurrent pneumothoraces.’
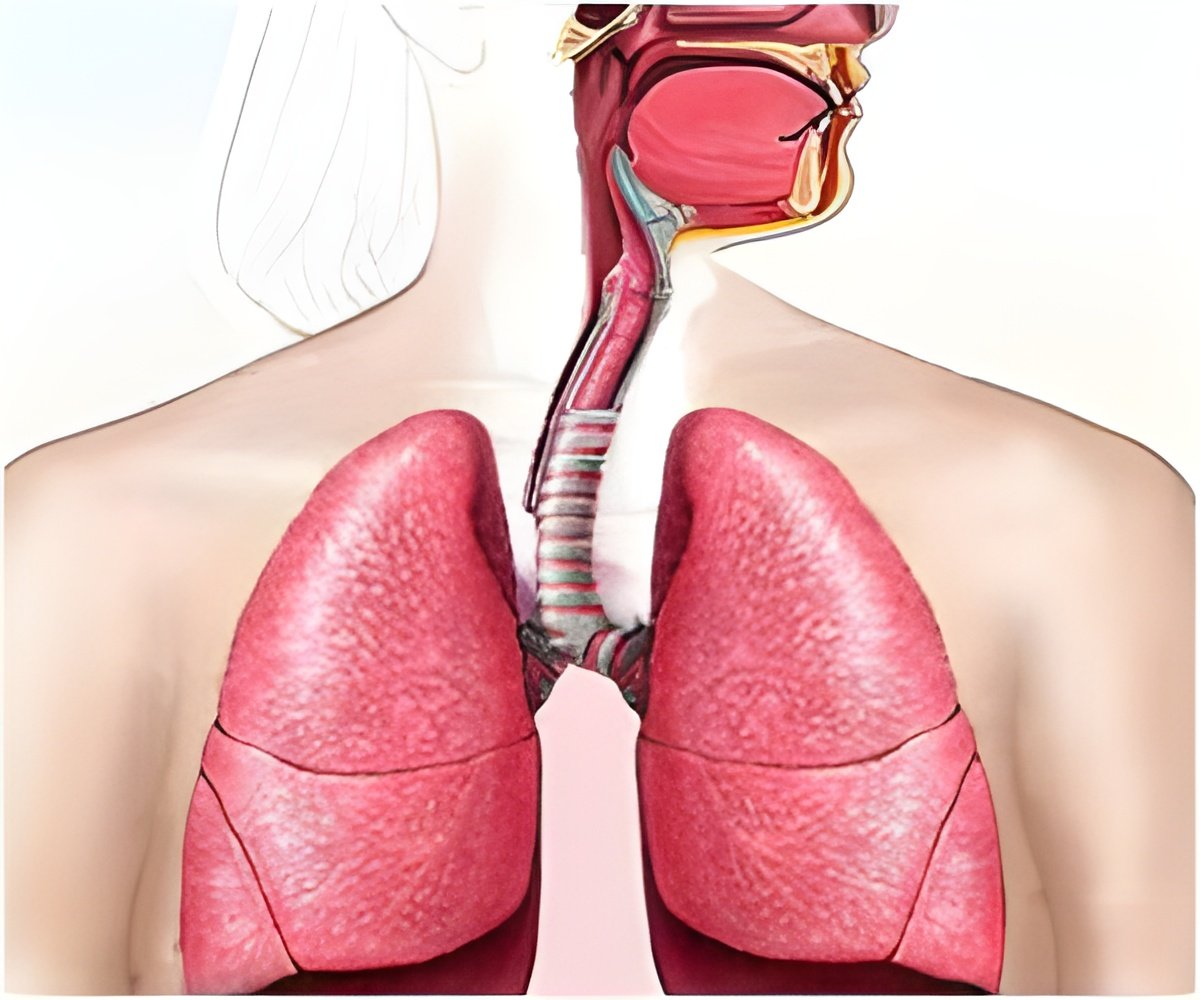
is a systemic disease that affects about five out of every million women. In patients with LAM, neoplastic smooth muscle-like cells arise from an unknown source, infiltrate the lung and result in cystic changes. Lung function declines at two to four times the normal rate, often punctuated by repeated lung collapses. Most patients are breathless with daily activities and require supplemental oxygen within 10 years of onset of symptoms.
A 21-member multidisciplinary committee of clinicians and scientists made four recommendations. The strength of the recommendations and the quality of the evidence supporting them were rated using the Grading of Recommendations, Assessment, Development, and Evaluation, or GRADE, approach.
For patients with cystic changes in the lung characteristic of LAM on high-resolution computed tomography (HRCT) but who have no other features of LAM, the guidelines suggest NOT using HRCT finding in isolation to make a clinical diagnosis of LAM.
The authors write that sirolimus, which was recently approved by the FDA as the first drug to treat LAM, is associated with potential adverse effects and, therefore, "it is essential to have a firm diagnosis prior" to prescribing its use. (This is a conditional recommendation with low confidence in the estimated effects)
When a definitive diagnosis of LAM is necessary, the guidelines suggest a diagnostic approach that includes transbronchial lung biopsy prior to a surgical lung biopsy. The authors note that definitive diagnosis by transbronchial lung biopsy can eliminate the need for a more invasive surgical lung biopsy. (This is a conditional recommendation with very low confidence in the estimated effects).
After their first pneumothorax, the guidelines suggest that patients with LAM be offered ipsilateral pleurodesis rather than waiting for a recurrent pneumothorax before intervening with a pleural symphysis procedure. The authors note that early pleurodesis decreases the risk of recurrent pneumothoraces. (This is a conditional recommendation with very low confidence in the estimated effects)
The guidelines suggest that previous unilateral or bilateral pleural procedures NOT be considered a contraindication to lung transplantation in patients with LAM.
The authors base this recommendation on the studies that have shown that the patient outcomes following lung transplantation in patients with prior pleurodesis were not substantially different than the patients who had not undergone prior pleurodesis.
Similar to these guidelines, the International Society for Heart and Lung Transplantation recently stated that pleurodesis should not be considered a contraindication to lung transplantation and that patients should be offered the best immediate care for pneumothorax. (This is a conditional recommendation with very low confidence in the estimated effects.)
"We continue to adjust our guidelines to keep pace with the evidence from clinical research," said Joel Moss, MD, PhD, co-chair of the guideline committee and deputy chief, Pulmonary Branch of the National Heart, Lung and Blood Institute.
Advertisement
"Patients are individuals and clinicians look at their specific cases when making treatment decisions. Their awareness of the guidelines and of the level of confidence in the potential effects of any course of treatment informs a doctor's decision making, without constraining it. That is the key benefit to patients."
Francis X. McCormack, MD, co-chair of the guideline committee and director of the Division of Pulmonary, Critical Care and Sleep Medicine at the University of Cincinnati, said, "Our hope is that these additional recommendations regarding diagnostic approach and pleural disease management can help protect patients from inappropriate drug exposures, unnecessary surgical procedures and recurrent pneumothoraces."
Advertisement
Nishant Gupta, MD, first author of the guidelines and assistant professor of pulmonary, critical care and sleep medicine at the University of Cincinnati, emphasized the need for more research. "The body of evidence the guidelines committee had to work with was small, and we identified several research directions that would greatly strengthen future recommendations," he said.
Among these were to:
Study the diagnostic accuracy of non-invasive methods when combined, such as HRCT plus clinical features of tuberous sclerosis complex, angiomyolipoma, chylous effusion, or lymphangioleiomyoma.
Determine the diagnostic yield of transbronchial lung biopsy in an unselected patient population, the relationship between disease burden and yield, and the optimal balance between diagnostic yield and risk of complications in patients, as well the safety and efficacy of two relatively new diagnostic tools: endobronchial ultrasound guided transbronchial needle aspiration and transbronchial lung cryobiopsy.
Identify the ideal method of achieving pleural symphysis in patients with LAM, "one which provides the optimal balance between efficacy of preventing future recurrences" and complications during lung transplantation.
Determine whether sirolimus and other mTOR inhibitors impact pneumothorax occurrence.
Ascertain whether outcomes following a bilateral lung transplant are better than a single lung transplant.Source-Eurekalert