‘Bruton's tyrosine kinase inhibitors could serve as potential new treatment option to reduce the risk of thrombocytopenia caused by heparin.’
Read More..Tweet it Now
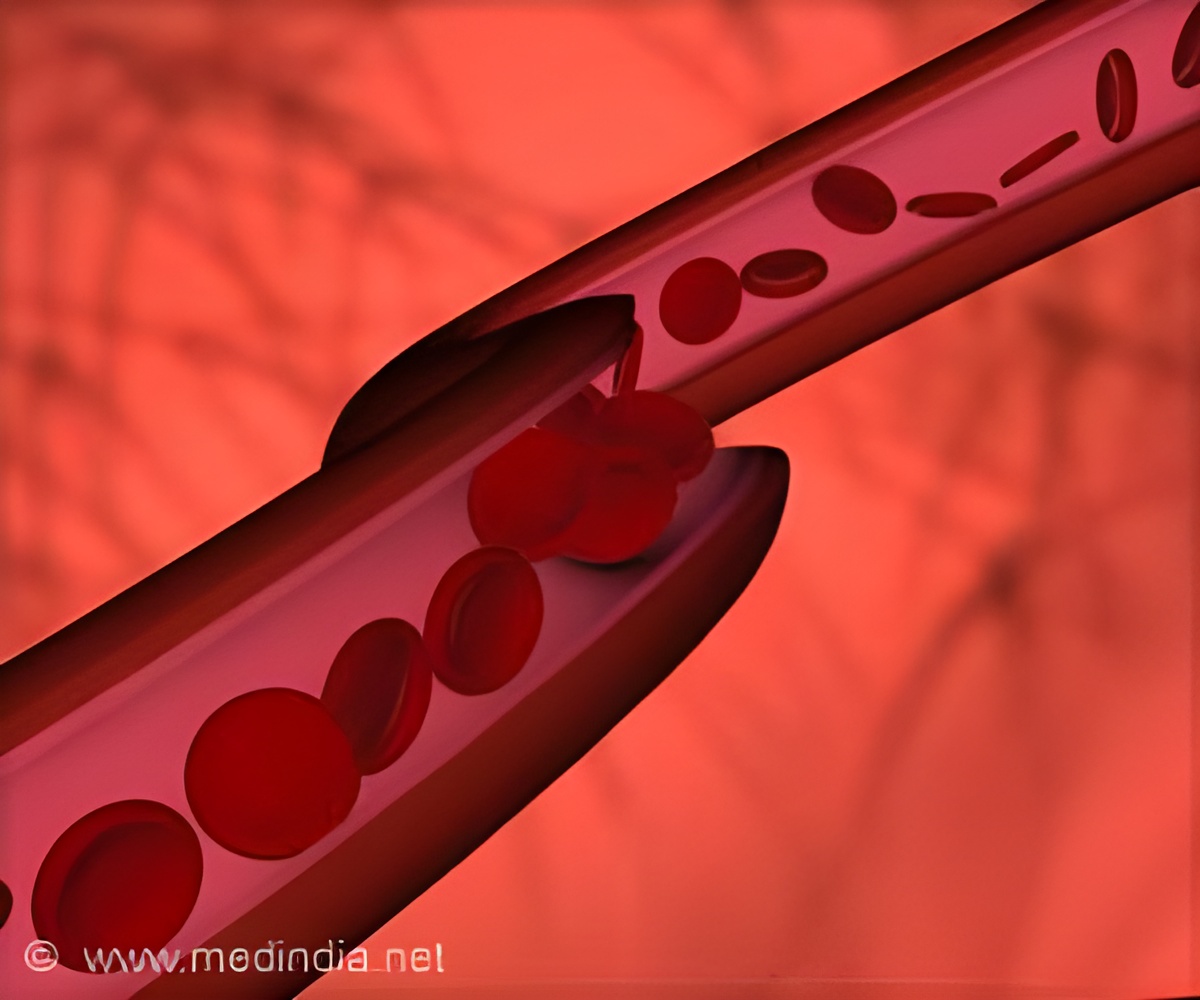
However, the agent can also lead to a reduction in the numbers of thrombocytes (otherwise known as platelets) in the bloodstream - an effect known as HIT. Up to 3% of patients who are treated with heparin develop an immunologically triggered subtype of HIT (called type II HIT), which is surprisingly associated with an increase in the incidence of thromboses (clots) in the blood vessels that are potentially life-threatening. Read More..
The incorporation of platelets into the blood clots explains the occurrence of thrombocytopenia. A new study directed by Wolfgang Siess, Professor of Cardiovascular Pathobiochemistry at LMU's Institute for Prophylaxis and Epidemiology of Cardiovascular Diseases (IPEK), has now demonstrated that this hazardous side-effect can be effectively prevented in vitro by the inhibition of a specific enzyme.
The discovery provides a new option for the treatment of type II HIT. The study was carried out in collaboration with research groups led by Professor Michael Spannagl (Department of Transfusion Medicine, Cell Therapeutics and Hemostaseology, LMU Medical Center) Professor Christian Weber and Dr. Philipp von Hundelshausen (both IPEK).
Heparin is a large, negatively charged linear polysaccharide made up of a variety of repeat units. Type II HIT is caused by the formation of antibodies that are directed against a specific molecular complex made up of heparin and a protein called PF4, which is secreted by platelets.
The so-called Fc domain of the antibodies binds to the corresponding Fc receptor found on the platelet surface, which results in activation of the cells.
Advertisement
This leads to the formation of thrombin and fibrin, and together with platelet activation triggers clot formation. - Hence heparin actually provokes the effect that it is intended to inhibit. "The complex pathogenesis of type II HIT is quite well understood, but the standard therapy of the disorder is suboptimal," says Siess.
Advertisement
We found that each of the six Btk inhibitors we tested was indeed able not only to reduce but to completely block Fc-receptor induced platelet aggregation and secretion in blood. In addition, they all blocked the interaction of thrombocytes with neutrophils - thus preventing the formation of potentially harmful thromboses," Siess explains.
"This was a very pleasant surprise for us, as earlier investigations had shown that Btk inhibitors could only partially block platelet activation induced by stimulation of a different receptor."
Inhibitors of Btk therefore offer a new promising therapeutic option for type II HIT, as they target an early and crucial step in the process that gives rise to the disorder. The inhibitors employed in the study have the additional advantage that they have either been approved for the treatment of other diseases, or have been successfully tested in clinical trials.
Source-Eurekalert