‘Along with increasing donor options, immuno-suppressing drug combinations have the potential to address racial disparities in stem cell transplantation.’
Tweet it Now
Although the treatment is successful for many, half of those who undergo the procedure experience some form of graft-versus-host disease (GvHD). Most cases of GvHD are treatable, but an estimated one in 10 can be life-threatening.Graft-versus-host disease (GvHD) happens when the newly implanted immune cells recognize their host’s body as “foreign” and then target it for assault, much like they would an invading virus.
Immune-suppressing drugs are used to prevent GvHD by the donated cells, and mostly unrelated patients are matched whenever possible with donors beforehand to make sure their immune systems are as similar as possible.
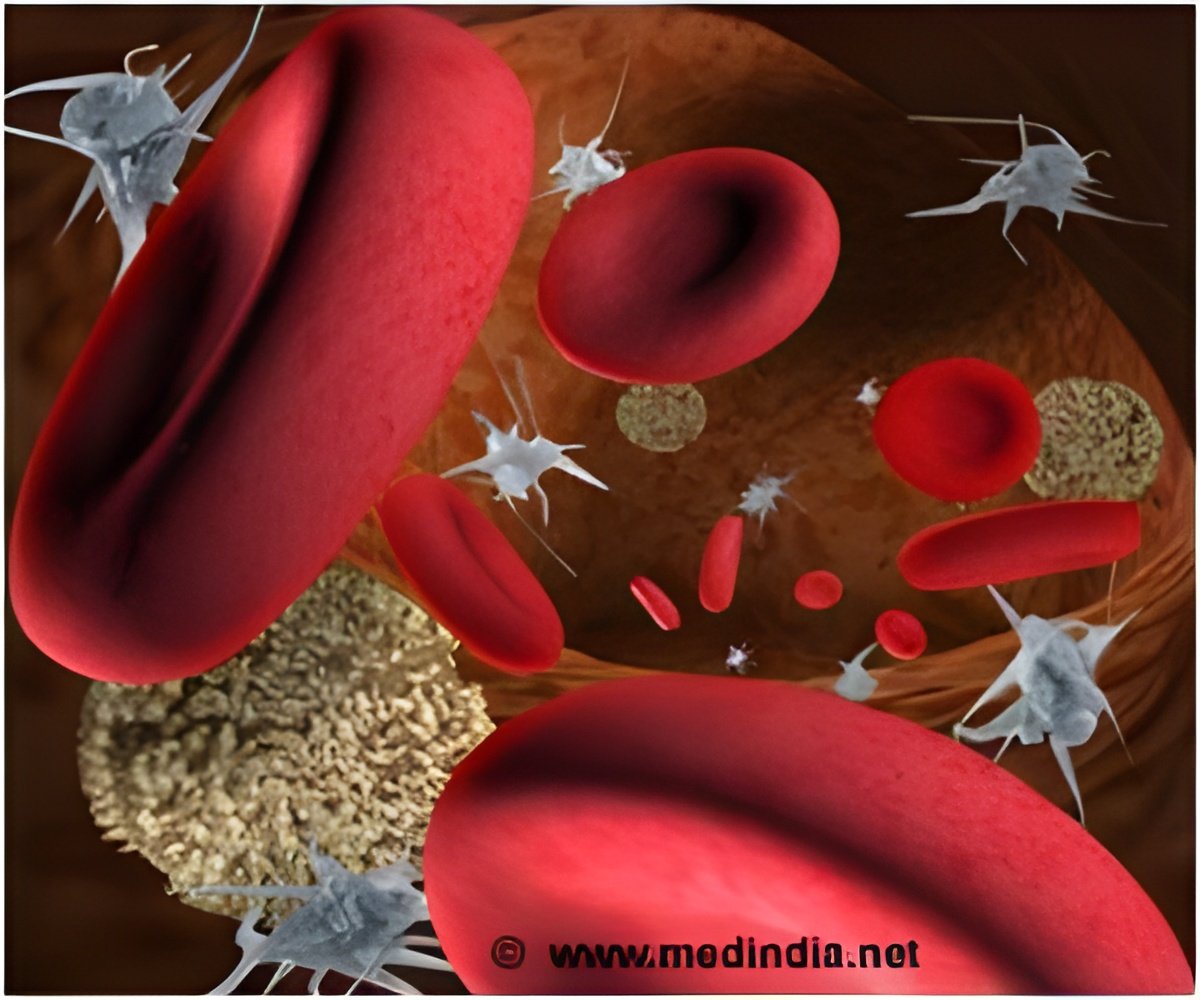
A new study better addressed the problem of GvHD in people being treated for blood cancer using abatacept in combination with other immune-suppressing drugs is both safe and an effective means of preventing GvHD after stem cell transplantation for blood cancers.
“The signs of GvHD with abatacept were minimal and treatable. None were life-threatening,” says Al-Homsi, a clinical professor in the Department of Medicine at NYU Grossman School of Medicine and Perlmutter Cancer Center.
Advertisement
The study showed that among the first 23 adult patients with aggressive blood cancers given the posttransplant drug regimen over three months, just four showed early signs of GvHD, including skin rash, nausea, vomiting, and diarrhea.
Advertisement
None developed more severe symptoms, including liver damage or difficulty breathing. However, one patient, whose transplant failed, died of recurring blood cancer.
The rest (22 men and women, or 95 percent) remain cancer-free more than five months after their transplant, with donated cells showing signs of producing new, healthy, and cancer-free blood cells.
The current study involved stem cell transplantations from closely related (half-matched) donors and patients, including parents, children, and siblings, but whose genetic make-up was not identical, with the drug combination increasing the likelihood of successful transplantation.
By improving the odds against developing graft-versus-host disease, the pool of family members who can safely serve as stem cell transplant donors for people with blood cancers, regardless of their ethnic background can be expanded.
Source-Medindia