Highlights
- Microbes living in the reproductive tract can help identify pregnant women who are at risk of giving birth prematurely
- Subtle changes to the vaginal bacteria can lead to premature birth
- Decrease in the levels of Lactobacillus bacteria and increase in other types of bacteria can lead to premature birth
Link between Bacteria and Premature Birth
In this study, the research team revealed that a shift away from the usual healthy balance of vaginal bacteria was linked to the waters breaking early, and can create an enormous impact on the health of mother and baby like increasing the risk of sepsis for newborns.
In a paper that was published in the journal BMC Medicine, the research team highlighted that while the standard antibiotic treatment (prescribed by national guidelines) given to women whose waters break early can help to reduce infection. However, for a small subset of women, it could be detrimental.
The team also explains that for a small subset of women the treatment, administered as a protective measure in hospital, can disrupt the balance of the mother's microbes by eradicating the 'good' bacteria and allowing more harmful bacteria to take their place in the vagina with potentially devastating consequences for the baby.
The research team suggested that alternative treatments are required for these women to reduce their risk.
Premature Rupture of Membrane
Babies are protected inside the amniotic sac during pregnancy that is surrounded by the membrane rupture as part of the normal birthing process when the mother's 'waters break' one hour before labor. However, when this occurs before 37 weeks, the baby is born prematurely and is termed as Premature rupture of membrane (PPROM).
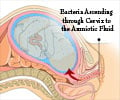
After the membranes rupture, the baby remains without the protective membrane and is at higher risk of infection as the vaginal bacteria spread upwards to the placenta and uterus. The women whose waters are broken early are usually given intravenous antibiotics to reduce the risk as a standard practice on the NHS.
The research team from the Institute of Reproductive and Developmental Biology (IRDB) at Imperial observed the impact of premature rupturing of the membrane and antibiotic treatment on the vaginal microbiota by taking swabs from the vaginas of pregnant women at different points during their pregnancy and analyzed them to reveal the different types of bacteria present, their proportions and any changes.
Findings of this Study
The samples were collected from about 250 pregnant women who were with and without risk factors for giving birth prematurely like family history of preterm birth or miscarriage. About 27 of them had a premature birth.
The research team also collected samples from a second, smaller group. There were about 87 women who were at the hospital with premature rupture of membranes.
All the patients were from Queen Charlotte's and Chelsea Hospital and Chelsea and Westminster Hospital.
In a previous study, over the course of pregnancy, the bacteria that colonize the vagina becomes less diverse and are dominated by Lactobacillus species, which can be found in the body like the gut and mouth.
The research team analyzed the samples, and the results show that premature rupture of the membrane was linked to a shift in the microbiota, with a drop in Lactobacillus and an increase in other types of bacteria, including potentially harmful bugs like Staphylococcus and Streptococcus.
The samples taken from the small group of women with premature rupture were analyzed before and after the preventative antibiotic treatment. Oral erythromycin was given four times a day for ten days. Before treatment, the swabs were taken and then at 48 hours, and then after one week and two weeks.
For those women whose microbial makeup was dominated by Lactobacillus before the treatment, the results showed that antibiotics declined in Lactobacillus and increased the diversity of bugs.
In those women who had reduced Lactobacillus, the treatment was beneficial in some of them, where the amount of potentially harmful bacteria decreased.
Antibiotic Treatment
In this study, the research team also revealed the link between specific vaginal bacteria and newborns who developed sepsis after delivery.
Mothers of healthy babies dominated lactobacillus, and the samples from the mothers of newborns with sepsis showed a greater diversity of bacteria like even the presence of Streptococcus and E. coli.
Dr. David MacIntyre who is from the Imperial IRDB said that this is one of the first studies to show that about a half of pregnant women could have an unbalanced vaginal microbiota before premature rupture, providing further evidence of the role of bacteria in some cases of premature births.
“Crucially, our findings identify two different groups of women with premature rupture one group in which targeted antibiotics may be beneficial and the other in which this same treatment may be detrimental," said Dr. David MacIntyre.
Need for Further Study
Further research is needed to assess current clinical guidelines available for women with premature rupture, and developing alternative treatments like using more selective antibiotics can help improve outcomes for women and their babies.
Professor Phil Bennett, a Professor of Obstetrics and Gynaecology at Imperial said that every woman in this study was treated with national and hospital guidelines, which shows that there is an urgent need to investigate if these guidelines are appropriate and effective.
He also said that these findings could play an essential role in the use of antibiotics as a preventative measure for these women. In the UK and other countries like Canada, Australia, Germany, and New Zealand this course of action is recommended.
"The aim of antibiotic treatment in PPROM is to reduce the risk of ascending infection. Our results suggest that a more personalized approach targeting only those women likely to benefit from antibiotics may prove more beneficial than the current 'one treatment fits all' approach," added Dr. Richard Brown, a Clinical Research Fellow at Imperial and first author of the study.
Source-Medindia