Highlights
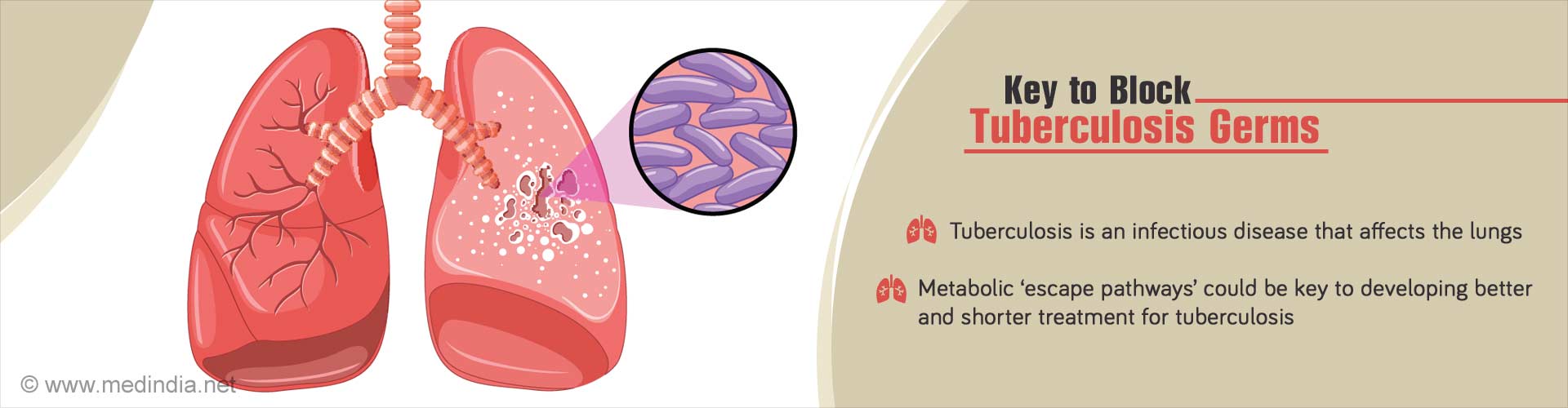
- Tuberculosis caused by Mycobacterium tuberculosis is an infectious disease that usually affects the lungs.
- Anti-tubercular drugs used for treatment are often linked to poor compliance, longer duration of therapy and side effects.
- Blocking the Tuberculosis germs by metabolic “escape pathways” could be a new key for a better and shorter treatment.
A research study from the Oregon State University scientist Luiz Bermudez has estimated that decreasing the duration from 6 months to three weeks could likely eliminate poor compliance.
The research study would also be a new key to developing a shorter therapy for tuberculosis.
Why is it difficult to follow a Long term tuberculosis treatment?
Tuberculosis treatment can be difficult to follow due to
- Side effects of TB drugs
- The disease being more prevalent in impoverished countries
- Lack of essential medicines as patients often live great distances from pharmacies and other medical facilities
The research team has taken a biology-driven approach to learn how the Mycobacterium tuberculosis could prolong survival following the exposure to different antimicrobial concentration.
The research team investigated on how the Mycobacterium tuberculosis bacteria could react to each class of anti-tuberculosis drug. So, that a more reasoned combination therapy could be developed.
The responses of the bacteria to the five compounds were studied:
- Isoniazid
- Rifampicin
- Moxifloxacin
- Mefloquine
- Bedaquiline
Bermudez said, "When we looked at the enzymes carefully, we realized the enzymes being synthesized by the bacteria were enzymes connecting several different metabolic pathways."
"Then we came up with the idea that maybe what the bacteria were trying to do, in the presence of a bactericidal compound that was threatening their way of living, was use other ways to survive. One of the things we saw, for example, was a shift to an anaerobic metabolism, which makes a lot of drugs inactive and incapable of killing bacteria.”
He also added that, the gene inactivation of some of the enzymes could improve the drug efficacy against Mycobacterium tuberculosis.
The identified proteins could also provide powerful targets for developing synergistic drugs that are aimed to accelerate bacterial killing.
Using a combination of drugs to treat tuberculosis may also be an attempt to prevent antimicrobial resistance.
However, antibiotics in some cases could antagonize the effects of each other. Therefore, by using another compound that could inhibit the bacteria from shifting the metabolic pathways could help to get a more reliable and desirable synergy of therapy. And also produces a significant impact on reducing the time that is needed for therapy and improves compliance. This could also reduce the emergence of resistance.
Interesting Facts on Tuberculosis
- Tuberculosis is considered to be one of the top three causes of death among women.
- Childhood tuberculosis is estimated to make up about 8% of global incidence of tuberculosis.
- People who are recently infected with tuberculosis bacteria and those who have a weakened immune system are at a high risk of developing tuberculosis.
- Tuberculosis could be a serious health threat for people who are infected with HIV.
- Lia Danelishvili et al, proteome response to anti-tuberculosis compounds reveals metabolic "escape" pathways that prolong bacterial survival, Antimicrobial Agents and Chemotherapy (2017). DOI: 10.1128/AAC.00430-17
- TB Quick Facts - ( http://www.treatmentactiongroup.org/tb/resources/tb-quick-facts)
- Basic TB Facts - ( https://www.cdc.gov/tb/topic/basics/)
Source-Medindia