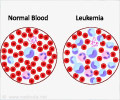
- The leakiness of blood vessels of the bone marrow in acute myeloid leukemia reduces the delivery of chemotherapy drugs
- This could result in resistance to treatment and relapses
- The leakiness can potentially be improved with the concomitant use of nitric oxide synthase inhibitors
Scientists conducted studies in mice to get a better insight into the disease process of AML and came up with treatment options that could improve outcomes. The scientists found that:
The blood vessels of the bone marrow in mice with AML show variations in structure and function. The bone marrow blood vessels were highly leaky. The increased leakiness of blood vessels could result in reduced delivery of chemotherapy drugs to the bone marrow, and therefore reduced effectiveness of the treatment.
Hypoxia, or reduced oxygen level, was present, while the levels of nitric oxide were high. The high nitric oxide level was a probable reason for the increased leakiness of the blood vessels. Nitric oxide is a small signaling molecule secreted by the endothelial cells, the cells lining the inner aspects of blood vessels. The molecule is formed through a reaction mediated by an enzyme called nitric oxide synthase. It relaxes blood vessels and reduces blood pressure. It is also involved in several other physiological processes like neurotransmission and immune system reactions, and pathological processes like septic shock, neurodegenerative disorders and acute and chronic inflammation.
Nitric oxide synthase inhibitors improved the response to treatment with the anticancer drug cytarabine. Nitric oxide synthase inhibitors reduce the level of nitric oxide and are already being evaluated in clinical trials for various other conditions. The progression of the cancer slowed down and it did not recur for a longer duration in the mice who received both the drugs as compared to those mice who were administered only cytarabine. The inhibitors reduced the leakiness of the blood vessels, which suggests that the leakiness was due to high nitric oxide levels.
Thus, if cytarabine is given along with a nitric oxide synthase inhibitor, the inhibitor could possibly improve the response to cytarabine, by improving the drug delivery to the cancer cells and thereby reducing the chances of treatment failure and relapses. Further studies, in humans are required before such an approach could be adopted in clinical medicine.
- Passaro D et al. Increased Vascular Permeability in the Bone Marrow Microenvironment Contributes to Disease Progression and Drug Response in Acute Myeloid Leukemia. Cancer Cell. DOI: http://dx.doi.org/10.1016/j.ccell.(2017).08.001