- The World Health Organization (WHO) initiates a global study to address the problem of medication errors
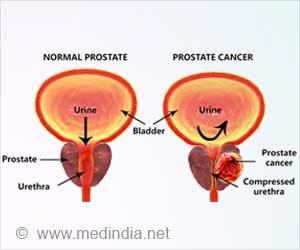
- Patients with abnormal kidney and blood clotting functions had a higher number of severe errors
- Therefore, the prescription should be correct regarding the dose, frequency, route, and duration of the drug to be taken
Read More..
What are Prescription Errors?
A prescription error means the failure of the process of prescription writing or documentation that results in wrong instructions about one or more of the normal features of a prescription, like the date of the prescription, patient identification, and the correct drug with complete instructions on its use (1✔ ✔Trusted SourceWHO launches global effort to halve medication-related errors in 5 years
Go to source).
Since prescription errors are the most preventable, this study was conducted with the primary aim of determining the incidence of medication errors in ICU patients in a tertiary care teaching hospital.
This study recorded the rate of errors during the prescribing phase of the medication process, conducted from January 1 to June 30, 2018, in the ICU of an academic tertiary care hospital in North India. All patients admitted to the ICU for more than 24 hours were included in the study after obtaining consent from their attendants.
Baseline characteristics, including demographic data (name, gender, age, weight, height, and admission number), diagnosis, and health evaluation at 24 hours of admission, were recorded. Further data, such as the total number of days of mechanical ventilation, the number of days of ICU stay, the outcome, and mortality in ICU, were also acquired.
Prescription errors were identified if the treatment chart mentioned wrong spelling, wrong dose, wrong route of administration, or wrong frequency of administration of any drug. The daily treatment chart for each patient was considered a separate entity. Each drug in the chart was evaluated against standard prescriptions regarding dose, frequency, and route.
Medication Errors at a Tertiary Hospital Intensive Care Unit
Out of a total of 24,572 medication orders, 2,624 had prescription errors. A total of 867 MPEs (Medication prescribing errors) required interventions or resulted in patient harm, and 1,757 MPEs did not result in patient harm. Approximately 70% of the severe MPEs occurred in the antibiotics group alone. Although general care and nutrition constituted the highest number of MPEs, nearly 91% of these were non-severe (2✔ ✔Trusted SourceMedication Prescription Errors in the Intensive Care Unit: Prospective Observational Study
Go to source).
Despite daily feedback as per our protocol, the errors in the prescription of these drugs (especially missing dose/route of administration) persisted. Another important finding is that patients with raised creatinine had twice the chance of having severe MPEs.
Once the need for renal replacement therapy arises, the dose of antibiotics needs further modification, sometimes daily, depending upon the method of kidney replacement therapy.
Patients with extended ICU stay had more MPEs, which we believe merely represents the fact that a longer ICU stay leads to more drug prescriptions and more errors, as shown in an earlier study that found days of hospital stay and mechanical ventilation, and the number of prescribed drugs positively correlate with the number of MEs.
As this study was a single-center study in a tertiary care academic hospital, the results may not be generalizable. After the identification of errors, feedback was given to the treating doctors daily. This might have reduced the probability of similar errors until the same team of doctors was posted in the ICU.
Another limitation of this study is that MPEs for drugs administered as continuous infusions were not analyzed. Due to the dynamic titration of drugs in infusion, researchers decided to omit these drugs for detecting MPEs.
Detecting MPEs with direct chart review and total sampling is an important strength of the study. Also, as the same team recorded all observations, interobserver variability, and undetected errors are expected to be minimal. Focusing only on the numbers and severity of prescription errors provides an opportunity to adopt practices targeting the reduction of these errors in critically ill patients.
The availability of the incidence of MPEs in acute kidney injury and deranged coagulation profiles will help improve the quality of care and reduce MPEs to a minimum. A larger study to analyze all forms of drug errors occurring during the mediation process may be planned in the future.
This observational study demonstrated the incidence of prescription errors in a medical ICU at a tertiary care hospital to be 10.7%. However, only 3.5% were severe errors that required interventions or resulted in patient harm. This incidence can be reduced further with sensitization, training, monitoring, and reinforcement.
Preventing Medication Errors in Critical Care
Moreover, due to the complexity of clinical settings and the sources of MEs, it is recommended not only one intervention to prevent medication errors but rather an integrated system that includes several safety barriers that allow for the prompt identification of anomalous processes; such barriers should intervene to protect the system from possible damage and contain the negative consequences of anomalies (3✔ ✔Trusted SourceMedication errors: prescribing faults and prescription errors
Go to source).
Vigilance on the part of nurses and the adoption of precautionary measures regarding medication errors in ICUs are key factors in preventing medication errors.
Strategies that Yield Positive Effects in a Clinical Practice
The following steps help in ensuring proper clinical practice- The creation of a safe environment for medication preparation by placing labels.
- The reduction in distractions and interruptions during medication administration
- The mandatory double-checking of medications
References:
- WHO launches global effort to halve medication-related errors in 5 years - (https://www.who.int/en/news-room/detail/29-03-2017-who-launches-global-effort-to-halve-medication-related-errors-in-5-years)
- Medication Prescription Errors in the Intensive Care Unit: Prospective Observational Study - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9160616/)
- Medication errors: prescribing faults and prescription errors - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2723200/)
Source-Medindia