‘Customizing the blood thinner to a patient's genetic profile helps determine the optimal dose, reducing the risk of bleeding, blood clots, and warfarin overdose.’
Tweet it Now
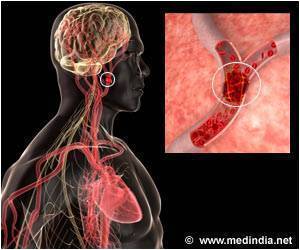
Despite its decades-long use, determining the correct dose can be difficult. The drug affects people differently, and genetics come into play. Too much warfarin can cause internal bleeding, while an inadequate dose fails to prevent blood clots. Over the last 10 years, warfarin has led to more medication-related emergency room visits among older adults than any other drug.The new warfarin study, published in the Journal of the American Medical Association, found that customizing the blood thinner to a patient's genetic profile helps determine the optimal dose, reducing the risk of major bleeding, blood clots and a warfarin overdose.
"Warfarin is very effective in preventing blood clots, but it's very difficult to regulate," explains Anne R. Bass, MD, a rheumatologist at Hospital for Special Surgery (HSS) in New York City and study co-author. "About half of the population, because of genetic variants, is very sensitive to warfarin or has a very unpredictable or delayed response to the drug. This is the first study to show that adjusting the dose based on these genetic variants makes warfarin safer for patients."
The multicenter clinical trial, known as GIFT (The Genetic Informatics Trial of Warfarin to Prevent Deep Venous Thrombosis) was funded by the National Institutes of Health. Brian F. Gage, MD, a professor of Medicine at Washington University School of Medicine, served as principal investigator. Hospital for Special Surgery had the highest number of study participants -- almost 1,000 joint replacement patients.
Investigators collected data on a total of 1,600 individuals age 65 and older undergoing hip or knee replacement surgery. Patients were randomly assigned to one of two groups. One group received warfarin dosing based on clinical factors known to affect warfarin dose such as age, height and weight, gender, race, and other medications; the second group's dose was based on these factors plus genetic variants. The study zeroed in on genetic variants in three genes, and this genetic information helped guide warfarin dosing during the first 11 days of treatment.
Advertisement
Dr. Bass adds that although the study involved joint replacement patients, the findings have implications for other populations taking warfarin. "This was really a study addressing warfarin management and warfarin safety, so I think you can extrapolate the results to other patients taking this blood thinner, such as those with atrial fibrillation," she notes. "A patient's genetic information is most valuable when you're initiating warfarin treatment."
Advertisement
Source-Eurekalert