Stroke patients in the US admitted during nights and week ends are at a higher rate of risk of death than those admitted during week days and business hours.
Stroke patients who enter the hospital at night and on weekends are more likely to die in the hospital than those treated during regular business hours and on weekdays, according to two studies presented at the American Heart Association’s International Stroke Conference 2008.However, regardless of when a symptom may occur, the American Stroke Association urges anyone who may be experiencing stroke symptoms to seek emergency treatment immediately.
In one study (P540), researchers used data from 222,514 acute stroke admissions at 857 hospitals participating in Get With The Guidelines-Stroke (GWTG-StrokeSM) (an American Heart Association quality improvement program), between 2003 and 2007. Researchers found that stroke patients who arrived in the emergency department during normal business hours (7 a.m. to 6 p.m. on weekdays) had better outcomes than those who arrived after hours, said Mathew J. Reeves, Ph.D., associate professor of epidemiology at Michigan State University in East Lansing, Mich.
“We found an elevated risk of in-hospital mortality for all stroke patients who presented after hours, but it was particularly striking for hemorrhagic stroke,” he said.
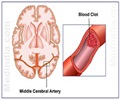
Hemorrhagic strokes are caused by bleeding into the brain. For the 34,845 hemorrhagic stroke patients in the final analysis, in-hospital mortality was 27.2 percent for off-hours presentation compared to 24.1 percent for those who arrived during regular hours.
“For hemorrhagic stroke patients presenting during off-hours there was a greater than 3 percent absolute increased risk in mortality,” Reeves said. “That’s clinically important; it translates to one excess death for every 32 patients with hemorrhagic stroke who present during off hours compared to those who arrive during regular hours.”
Advertisement
In a separate study (P174) – the largest study in the world to compare outcomes for weekend to weekday stroke admissions – California researchers analyzed data on more than 2.4 million hospital admissions throughout the country between 1988 and 2004 in which the primary diagnosis was stroke.
Advertisement
Using data from the U.S. government’s Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, Liebeskind and colleagues also found a difference, though less pronounced than for hemorrhagic stroke, between weekday and weekend admissions for patients who had an ischemic stroke. For those cases, mortality was 7.3 percent for weekday vs. 8.2 percent for weekend admissions, said Liebeskind, associate professor of neurology and associate director of the University of California Los Angeles Stroke Center.
The researchers theorized that patients who arrived in off hours period and on weekends might have different characteristics than those who arrive during regular hours and on weekdays. However, the differences in outcome persisted even after Liebeskind’s group adjusted for age, race, gender, and socioeconomic variables.
Reeves’ group adjusted for age, race, gender, stroke risk factors, arrival mode (personal vehicle or ambulance) and hospital-level factors and also found that accounting for these made little impact on the effect of off-hours arrival. While as yet undefined patient characteristics could still have had an effect, none were identified.
“The stroke patients admitted off hours have a higher mortality rate, and this cannot be explained by any obvious differences in characteristics of the stroke or the patient. This means that the reason may be a differences in the quality of care being provided by the hospital during these different times,” Reeves said, adding that this is the bright spot in the findings.
“If this is related to the quality of care then this could be fixable. It means that if hospitals look at their staffing and care practices on weekends and off hours, one should be able to correct these differences.”
Compared to ischemic stroke care, hemorrhagic stroke – which is caused by bleeding into the brain – carries a greater burden for specialist care such as neurosurgical interventionalists and neurosurgeons, he said.
“It could be that specialists are unavailable or more difficult to get hold of, and there’s definitely less staffing in terms of nursing care and rapid access to certain procedures on the weekend,” Reeves said.
Liebeskind’s study found that although patients admitted on weekdays and weekends underwent a similar number of procedures, those in the weekend group underwent their first procedure almost a day later on
average: 2.65 days after admission compared to 1.76 days for those arriving on weekdays, he said.
Liebeskind said the differences in outcome persisted though overall stroke mortality decreased during the 15-year study period.
“It’s difficult to say based on our study exactly where these differences arise,” he said, adding that this study
ended in 2004, about the time stroke care underwent a major change in the United States with more hospitals being designated as primary stroke centers.
A Primary Stroke Center is a hospital-based center that provides acute stroke care based on evidence-based guidelines and has the ability to treat emergently with the clot-busting drug, tissue plasminogen activator.
“We hope to see how these patterns will change with implementation of both primary and comprehensive stroke centers,” Liebeskind said.
Get With The Guidelines-Stroke is a continuous quality improvement program created by the American Heart Association and its American Stroke Association division. GWTG-Stroke provides healthcare providers with evidence-based treatment guidelines at the point of care and allows hospitals to gather data and review feedback on how well they meet a variety of treatment goals to improve outcomes. GWTG-Stroke started with a pilot program in 2003 led by Reeves’ co-author, Lee H. Schwamm, M.D., associate director of Acute Stroke Services at Massachusetts General Hospital, Boston.
Reeves said this study, which includes data from 2003 through 2007, appears to show an encouraging trend in
these GWTG-Stroke hospitals.
“There is some evidence in our data that the magnitude of the mortality difference between on-hour and off-hour arrival lessens the longer a hospital has been involved in the Get With the Guidelines quality improvement program,” he said.
American Stroke Association Advisory Chairman Ralph Sacco, M.D. said the studies show there is still room to improve stroke treatment.
“Although we are improving our rapid treatment approaches for acute stroke and improving outcomes, these new studies suggest that we may have room for improvement for those cases who present during off hours,” Sacco said. “The outcome disparities, however, were greatest for hemorrhagic stroke patients for whom we have the least successful acute treatments to offer.”
Source-Eurekalert
SPH/C