Dr.Sunil Shroff, Dr. S.Venkat Ramanan
STRESS URINARY INCONTINENCE (SUI)
Definition:
It is the complaint of involuntary leakage on effort or exertion, or on sneezing or coughing.
Approach to a patient with SUI:
SUI is a fairly straightforward and simple diagnosis. It does not need any complex test to prove it. Once the diagnosis is obvious, then the
degree of bother is to be evaluated along with enquiry into the lifestyle of the patient.
If the patient is using only few pads per day and her social life is not being altered by this problem, then conservative treatment is started straight away. Patient should be told to do pelvic floor exercises diligently for 6-8 weeks before re-evaluation of the symptom.
If the patient’s social lifestyle is significantly affected or her work involves moderate degree of exertion (eg-Aerobic instructor), then a surgical management is to be considered straightaway. In this situation, a prior Urodynamics will help before invasive therapy.
Urodynamics in SUI:
Indications for UDS:
1) Prior to invasive treatment
2) History of mixed incontinence
3) In previously failed incontinence surgery where re-surgery is contemplated
4) Previous radical pelvic surgery
5) Associated obstructive voiding/abnormal post void residue
6) Associated neurologic disorders
Advantages of UDS prior to invasive treatment:
1) Confirmation of incontinence and its cause
2) Definition of detrusor activity during filling – to rule out poor compliance
3) Assessment of detrusor during voiding – to rule out obstruction or detrusor underactivity
4) Assessment of degree of sphincter weakness
Urodynamic procedure in SUI:
The urodynamic procedure has to be carried out either in sitting position or in standing position. In sitting position, if stress leak is not demonstrated, the patient is asked to flex and abduct one thigh to open the introitus. Patient has to be properly explained the need for this position and taken into confidence before proceeding further.
Urodynamic finding in SUI:
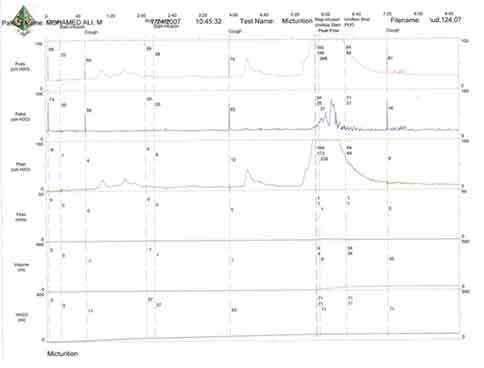
Urodynamic stress incontinence is the involuntary leakage of urine during filling cystometry occurring when the patient is asked to cough or do Valsalva manoeuvre.
The important finding to be noted is the increase in abdominal pressure (Pves or Pabd) without any detrusor contraction (ie – nil or minimal change in Pdet).
The volume at which the SUI occurs is to be noted. The Pves value at which the stress leak starts is also important.
Intrinsic sphincter deficiency is thought to be present if the stress leak occurs at Pves of less than 60cm H20.
Management of SUI:
The initial management of SUI includes teaching the patient a proper Keegel’s exercise, losing weight if obese and sometimes medication. The conservative approach is to be done for at least 6-8 weeks. If the patient continues to have significant symptoms affecting their social life, invasive treatment options are to be considered.
Mixed Urinary Incontinence:
Up to 12% women with apparently pure SUI can be shown to have Overactive bladder.
In mixed urinary incontinence, the frequency of SUI episodes is usually more compared to Urgency incontinence. However, patients are more likely to be troubled with urge urinary incontinence (UUI). This is because the UUI leak is a larger volume of leak leading to more pad usage and social embarrassment.
The initial management of mixed urinary incontinence is again conservative. It includes conservative measures as described for UUI along with pelvic floor exercises and drugs for OAB.
Urodynamics study is an invasive procedure causing considerable distress to the child and has an inherent risk of UTI and severe sepsis. Therefore it should be ordered only when other less invasive tests have not yielded the necessary information. Before an urodynamic study is performed, it is important for the child and the family to have full knowledge of the procedure. An explanatory leaflet should be provided so that parents will know what to expect and can explain the test to their child, or the child can read about it if he or she is old enough. A thorough history and clinical examination should be undertaken. Non invasive tests like uroflowmetry and ultra sonogram should always precede an urodynamic study in children.
Uroflowmetry
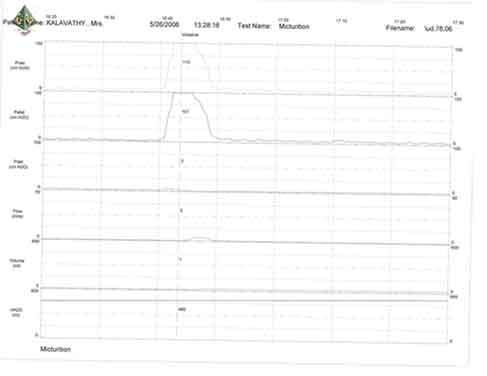
Uroflowmetry consists of measurement of urine flow during voiding and is described in terms of rate (ml/sec) and curve pattern. It is the least invasive of all urodynamic methods and is therefore perfect for paediatric use. However it requires a cooperative child, and is generally not possible in children less than 4 yrs of age. It measures urine stream during the emptying phase and gives an idea about bladder function and outlet function.
Age related uroflow nomograms are available separately for boys and girls depicting the maximum flow (Q max) in ml/sec. The normal curve pattern is ‘bell shaped’ or tower shaped some times and the flow ends usually within 10-15 sec (Figure 1). The normal Q max is generally above 10-15ml/sec. Values below 10ml/sec and a prolonged trace are suggestive of outlet obstruction, which may be anatomical (meatal stenosis, PUV) or functional (detrusor sphincter dyssynergia). Sometimes a staccato patter of uroflow is seen in these children with outlet obstruction. Over active bladder following prolonged obstruction causes a super normal curve while a lazy bladder causes a flat curve.
Uroflow can be combined with post void residual volume measurements to exclude obstructive uropathy. When combined with EMG, it becomes a very useful tool to assess sphincter incoordination. Uroflow EMG is becoming a norm in children with recurrent UTI and VUR these days to identify underlying dysfunctional voiding. It can also be used to provide biofeed back in dysfunctional voiders, to show how to relax the sphincters while voiding.
Indications for Urodynamics
Urinary incontinence in children can be mainly divided in to three etiological categories; neuropathic, uropathic and non neuropathic bladder sphincter dysfunction. The indications for urodynamics in children include
• Neurogenic bladder dysfunctions following
– Myelomeningocele, Spina bifida, sacral agenesis
– Pelvic surgery for anorectal malformations
– Transverse myelitis sequelae
– Sacrococcygeal teratoma and other spinal tumour excision
• Urinary outflow obstructions
– PUV, meatal stenosis following circumcision, Hypospadias
– Traumatic urethral strictures
• Intractable bladder dysfunction with
– Upper tract changes
– Renal functional impairment
Urodynamics in Children: Preparation
Rarely is any premedication given either orally or intramuscularly, but the child is conscientiously attended to in order to minimize his or her fears. If possible, the child is instructed to come to the urodynamic suite with a full bladder to obtain an initial representative uroflow. The child is catheterized with a 8F double-lumen urodynamic catheter after a small amount of liquid Xylocaine (1%) has been injected into the urethra and held in place for a moment or two.
Although urethral catheters are tolerated in newborns and adolescent children, children of the age group 3-10 find it very distressing and some times do not cooperate well. Once they start crying, it becomes difficult to obtain proper trace and artefacts start appearing. To circumvent this problem, it is becoming routine these days to insert suprapubic lines the previous day under GA. This is combined with a cystoscopy to assess the bladder status and exclude any obstructive pathology.
It is important to have rectal catheters to obtain a good abdominal pressure profile since children may cry, strain and cause a lot of artefacts during the procedure. To obtain a proper abdominal pressure the rectum must be empty. Since children with neurogenic bladder may also suffer from constipation it is essential to prescribe laxatives or enema for 2-3 days prior to the procedure.
Urodynamics in Children: Technical Differences
First, the intravesicular pressure is recorded. Then the bladder is drained and the residual urine is carefully measured. (Figure 2) Sometimes it is necessary to aspirate the catheter to get accurate information on the volume of residual urine. The rate of bladder filling per minute usually is selected by first calculating the child's predicted capacity and then dividing the result by 10 in order to fill the bladder slowly.
The average capacity in millilitres for a child older than 2 years of age is determined by Koff’s Formula. In younger children weight of the child is used to assess this.
Koff’s Formula: Volume (ml) = (Age + 2)30 ml
Fairhurst Formula: Volume (ml) = Wt(kg) x 7.5 ml
There are many other formulae to measure bladder capacity, however it is the author’s preference to use the above formulae due to its simplicity. It has been shown that more rapid filling rates may yield falsely low levels of detrusor compliance and may minimize uninhibited contractions in an attempt to avoid this problem, the bladder is filled slowly with saline warmed to 37°C. When it is important to determine very mild degrees of hyper tonicity, even slower rates of filling are used to measure its true incidence. During filling, it is helpful to try to divert the child's attention by asking unrelated questions, reading a story aloud, or showing a movie or cartoon. If the examiner wishes to elicit uninhibited contractions, the child is asked to cough; alternatively, a cold solution may be instilled at a rapid rate.
In most of the centres supine position is preferred for urodynamics in children. In adolescent and cooperative children, sitting position is possible. Video urodynamics is essential in children as most of them have associated VUR or sphinteric incompetence. Non compliance may be missed in these children unless simultaneous video is undertaken. Although needle EMG electrodes are the standard recommendation, EMG patch electrodes are equally informative and less traumatic. Simultaneous EMG recording is very informative in children with voiding dysfunction and neurogenic bladder.
Urodynamics in Children: Parameters measured
During Filling the following parameters are measured
Subscribe to our Free Newsletters!